- Empty cart.
- Continue Shopping
A Guide to Understanding Polycystic Ovary Syndrome (PCOS)
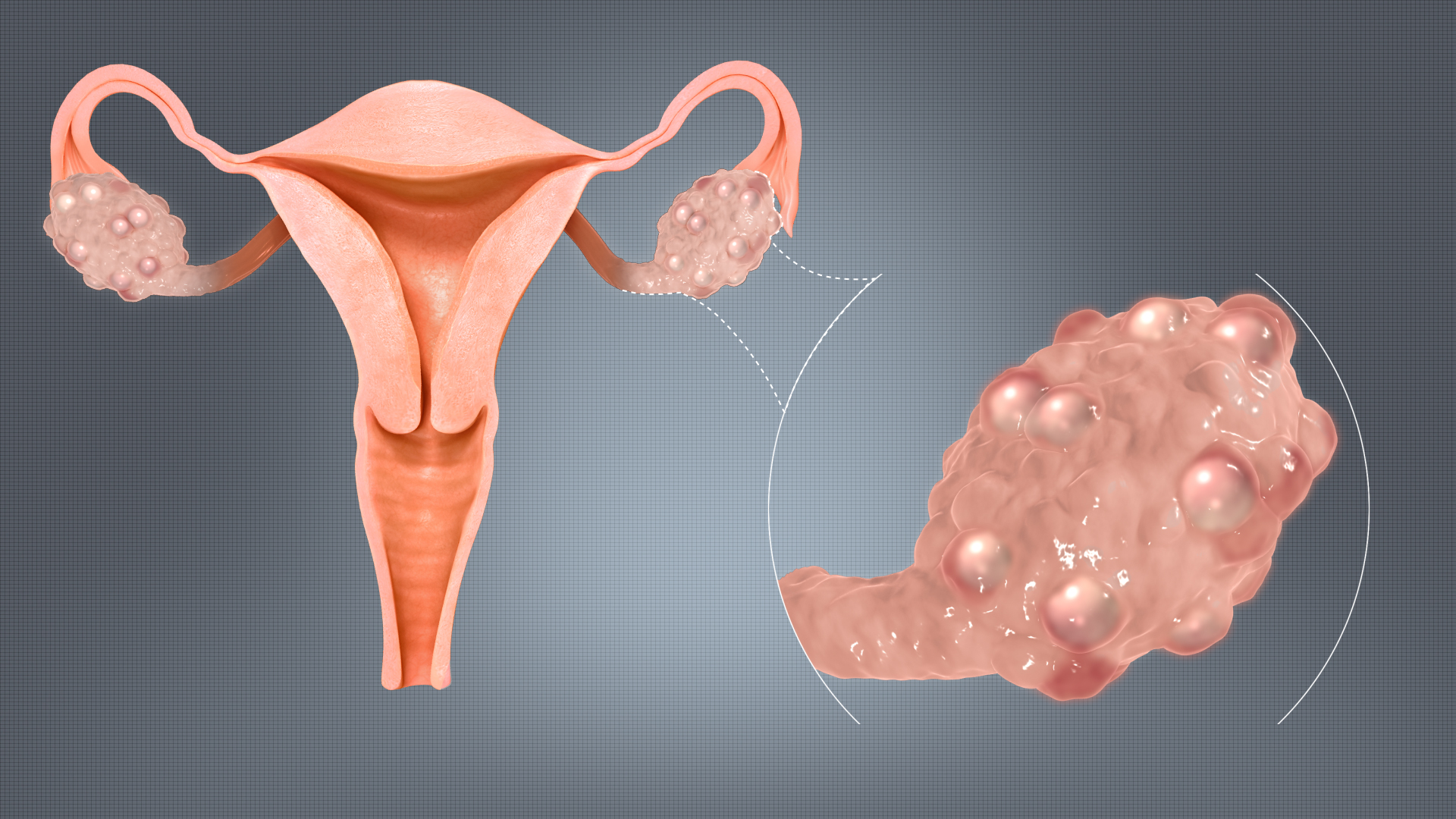
Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder that affects individuals with ovaries. It is characterized by a range of symptoms, including irregular menstrual cycles, elevated androgen levels, and the presence of small cysts on the ovaries. PCOS can have significant implications for reproductive health, metabolic function, and overall well-being.
1. Definition and Diagnosis
Polycystic Ovary Syndrome is a medical condition that involves a combination of hormonal imbalances and physical symptoms. Diagnosis is typically based on the presence of certain criteria, including irregular menstrual cycles, elevated androgen levels, and the appearance of cysts on ultrasound.
2. Common Symptoms
PCOS can manifest in a variety of ways, and the symptoms may vary from person to person. Common signs and symptoms of PCOS include:
- Irregular menstrual cycles
- Excess hair growth (hirsutism)
- Acne and oily skin
- Scalp hair thinning (alopecia)
- Weight gain and difficulty losing weight
- Mood changes and depression
- Pelvic pain
- Infertility or difficulty getting pregnant
3. Hormonal Imbalances
Individuals with PCOS often have higher levels of androgens, which are typically considered “male” hormones, but are present in both males and females. Elevated androgen levels can lead to symptoms like hirsutism, acne, and irregular menstrual cycles.
4. Metabolic Implications
PCOS is associated with insulin resistance, a condition in which the body’s cells become less responsive to insulin. This can lead to elevated blood sugar levels, and in some cases, the development of type 2 diabetes. Additionally, individuals with PCOS may have higher levels of cholesterol and blood pressure.
5. Reproductive Health
PCOS is a leading cause of infertility in individuals with ovaries. Irregular ovulation or lack of ovulation can make it more challenging to conceive. However, with proper medical management and lifestyle changes, many individuals with PCOS can achieve successful pregnancies.
6. Long-term Health Risks
Untreated PCOS can have long-term health implications. It is associated with an increased risk of developing conditions like type 2 diabetes, heart disease, and endometrial cancer. Regular monitoring and management of PCOS are crucial for mitigating these risks.
7. Management and Treatment
The management of PCOS typically involves a multidisciplinary approach that may include lifestyle modifications, hormonal therapy (such as birth control pills), and medications to address specific symptoms or conditions like insulin resistance. Weight management and regular exercise are also important components of treatment.
8. Emotional Well-being
PCOS can have a significant impact on emotional well-being. Dealing with the physical symptoms, infertility, and potential long-term health risks can be emotionally challenging. Seeking support from healthcare providers, therapists, and support groups can be valuable for coping with the emotional aspects of PCOS.
9. Lifestyle Considerations
Maintaining a healthy lifestyle is crucial for managing PCOS. This includes regular exercise, a balanced diet, and managing stress. Weight management, in particular, can play a significant role in improving symptoms and overall health.
10. Advocacy and Education
Advocacy and education are important aspects of managing PCOS. Raising awareness about the condition can help individuals with PCOS access the resources and support they need. Additionally, advocating for research and policies related to PCOS can lead to improved care and outcomes.
In conclusion, Polycystic Ovary Syndrome is a complex and multifaceted condition that requires careful management and individualized care. By understanding the various aspects of PCOS, individuals and healthcare providers can work together to develop effective treatment plans and support those affected by this condition in achieving optimal health and well-being.








